Rejuvenation Therapy – An Overview of Anti-Aging Stem Cell Therapies
Rejuvenation therapy is a form of medical treatment with the focus to halt, alter and even reverse the aging process. While there is currently no scientifically proven way to delay our internal aging processes themselves, there are ways to alter or delay some of the effects we experience as we age. Stem cell therapy is on the rise as a rejuvenation treatment. In this article, we discuss the differences between the various stem cell therapies for anti-aging.
What is Aging?
The biology of aging consists of several complex processes, many of which are not fully understood yet. However, scientists have discovered some processes that can explain why we age. In general, it can be said that the main aspects of aging are:
- Genetic aging, which can cause unstable DNA, mitochondria damage, cellular damage, telomere shortening or the inability for cells to reproduce sufficiently
- Biochemical aging, which is roughly the damaging of cellular structures through free radicals
- Hormonal aging, which is an increased impairment in our hormonal balance as we age
- Aging related to shortage of cellular resources, mainly lack of stem cells in tissue or oocytes
- Aging related to lifestyle choices, which can be understood as aging through external influences such as high sun exposure or smoking
All of these aspects play a role in aging, and some have a stronger effect than others. As the aging process is highly individual, the role of each of these aspects may be different in different individuals. This means that naturally, some people age faster than others.
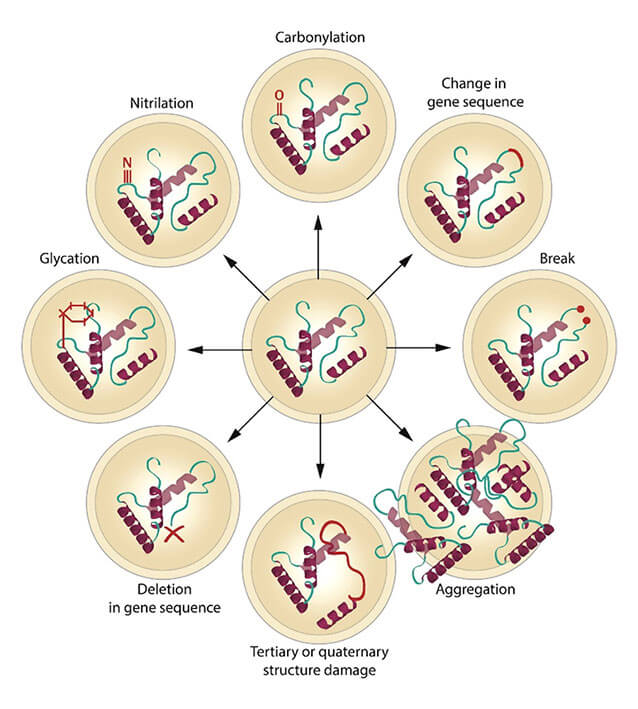
Figure 1: Examples of macromolecular damage. This example shows how a single protein can be affected by different damage types ¹.
Reversing Aging Effects by Replacing old or Diseased Cells
What is a logical way to stop aging? In the section above we listed some aspects of aging; most, if not all aspects are related to damage of cells or cellular structures. It makes sense to assume that the aging process could be altered by repairing those damages, or by completely replacing the affected cells with new, functioning cells.
The body naturally has many different mechanisms which it utilizes to repair molecular and cellular damages. However, these mechanisms not only decrease in functionality as we age, but also not every type of damage can be repaired. It is known that when organisms are unable to replace cells or at least dilute the damage, intracellular damage accumulates, which will have an effect not only on the functionality of the damaged cell, but also on its surroundings.
Indeed, the approach to replace damaged cells which the body cannot replace itself is being investigated for many different applications. Stem cell transplantation has been used for a while now, especially in the form of bone marrow transplants to treat serious diseases. Stem cell transplantation can also be used to treat type 2 diabetes by replacing brown fat cells. Stem cells can also be directly injected into the damaged body part, a technique often employed for orthopedic therapies, for instance to treat a fractured knee. As for examples for anti-aging applications, there are recent studies that were performed to enhance brain function or to reduce frailty.
Accelerating Healing Processes With Infusion Therapies
Stem cell infusion therapies are a novel approach within the stem cell treatment spectrum. Infused application can contain the stem cells themselves, or it can contain their “byproducts”. The idea came from fairly recent research which could show that the power of stem cells actually originates from their secreted products (such as miRNA, cytokines, proteins and growth factors) rather than the cells themselves. The sum of these secreted products are called secretome. Sometimes, the term “exosome” is used; that is, however, technically just one part of the stem cell secretome (read more about the differences here).
Just like stem cell-based therapies where the cells are directly injected, stem cell infusion therapies (with or without cells) can have different tissue origins. Scientific investigation currently explores all directions, from intravenous infusion of umbilical cord blood‐derived mesenchymal stem cells to intracoronary stem cell infusion after acute myocardial infarction.
The potential effects of stem cell infusion therapies are manifold; it can be anti-inflammatory, induce apoptosis in faulty cells, enhance the functionality of the immune system and activate healing processes which are naturally in place in the body.
Topical and non-Invasive Applications of Stem Cells
Another form of stem cell application is the topical solution. Instead of injecting the stem cells or applying them intravenously, a topical solution can directly be applied onto the skin. A therapy which is in high demand is the treatment of alopecia, or baldness. For such cases, stem cell therapy could be an effective alternative. A recent Korean study has shown very promising results of stem cell topical solution for baldness.
Another type of application is the stem cell therapy as a nasal spray. This can be a delivery method for the treatment of the brain, for instance in case of brain cancer or neurodegenerative diseases, without the need of a heavily invasive procedure.
Stem cells can also help in cases of chronic wounds, a major clinical problem which is also in high demand of therapeutic options. While still being investigated, this field of research is growing very quickly, because the potential of this application is so immense. This type of application is especially relevant for possible anti-aging treatments, which could make the treatment far more effective than the creams and lotions that are currently on the market.
Removing What’s bad – Senescent Cell Removal
When cells are not able to reproduce anymore, they will ideally commit suicide (called programmed cell death, or apoptosis) or they will shut down. These shut down cells are called senescent cells, and they are known to have a very high level of damage within themselves, which they accumulate during induction of senescence (initial insult‐inducing damage) and after senescence establishment due to an accelerated rate of damage accumulation.
Usually, senescent cells are removed by our immune system. However, as we age, this removal mechanism does not seem to work properly. As a result, more and more senescent cells remain in our body. These cells are not only internally damaged, but scientists have also found out that they are damage-inducing cells. This means that they “spread” the damage into their surroundings.
It is hypothesized that the elimination of senescent cells reduces the number of cells with the highest amount of damage. Some studies have shown overall improvement of health after senescent cell removal, such as improvement of heart, kidney, lung and adipose tissue function.
Another popular effect of senescent cell removal could be the activation and increased proliferation of hair follicle stem cells. In other words – it may be possible to treat hair loss, possibly with the combination of senescent cell removal and stem cell therapy, both of which could stimulate hair follicle activity.
Summary and Conclusion
There are different types of stem cell therapies:
- Stem cell transplantation or injection, where the cells are directly applied to the diseased or damaged area;
- Stem cell infusion therapies, where stem cells, or the stem cell secretome, are administered into the blood system;
- Topical or non-invasive stem cell therapies, where stem cells are applied as a topical solution, nasal spray or topical spray, and
- Cellular therapy through medication, the example discussed here being senescent cell removal.
There is no clear answer which type of approach is the most effective, because the effectiveness of the treatment depends on the treated person, the stem cell origin, and the disease to be treated.
A person who wants to regrow their hair may be interested in a topical treatment against baldness. If the main focus of the treatment is to enhance the immune system and accelerate healing processes from within, stem cell infusion therapy may be the application of choice. In the case of athletic performance enhancement, in particular in the field of orthopedics, a combinational therapy of stem cell injections and infusions, together with physical therapy, may be the way to go.
If you are interested to learn more about your options, contact us today. Our patient care managers will arrange a consultation with our expert physicians to discuss what approach may be the best for you.
References and Literature - Rejuvenation Therapy – An Overview of Anti-Aging Stem Cell Therapies
- 1. Ogrodnik, M., Salmonowicz, H., & Gladyshev, V. N. (2019). Integrating cellular senescence with the concept of damage accumulation in aging: Relevance for clearance of senescent cells. Aging Cell, 18(1), e12841.
